Results of the study of COVID in sub-Saharan Africa
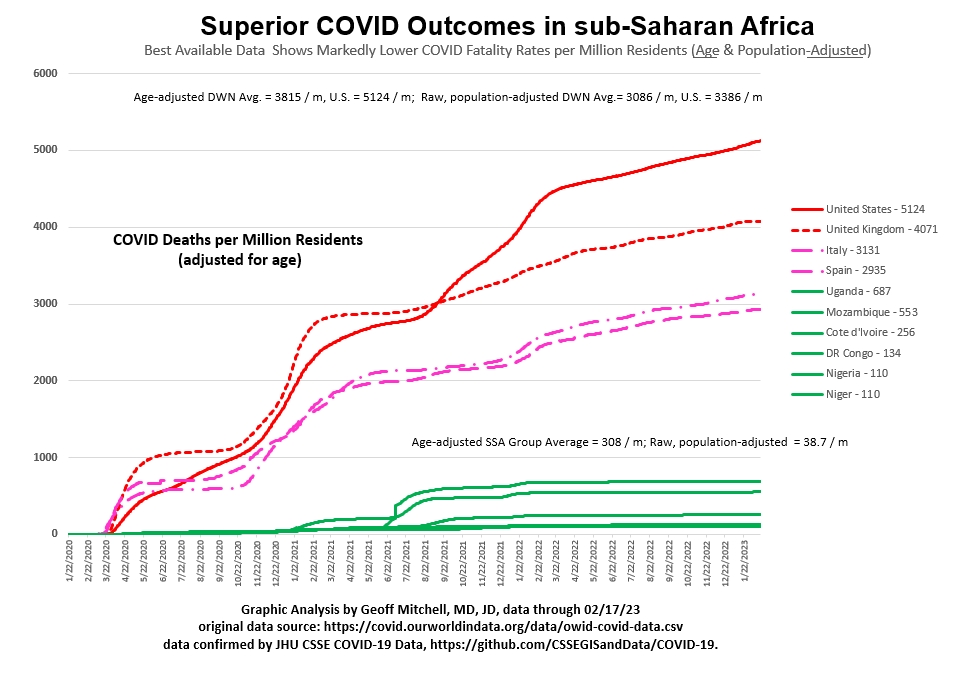
COVID fatality rate for SSA remains low and linear for three years.COVID fatality rate for SSA is about 7% of the rate for U.S. & Europe.COVID fatality rate for U.S. & Europe remains 23x that of SSA. |
|
As described in the studies section, an analysis was undertaken to test the hypothesis that malaria-endemic countries whose visitors were almost all taking hydroxychloroquine-like anti-malarial prophylaxis would have a lower incidence of COVD-19 fatalities. The first paper was produced on May 11, 2020. The initial data source was the "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University," aka the "COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University" or "JHU CSSE COVID-19 Data" for short, and the url: https://github.com/CSSEGISandData/COVID-19. Results of initial paper, ~ May 1, 2020. See the most current graph here. A similar confirmatory graph can be produced on the "Our World in Data" website, seen here. This was a study of the improved COVID-19 outcomes in malaria endemic sub-Saharan African ("SSA")countries compared to the U.S. and the industrialized West - "Markedly Lower Rates of Coronavirus Infection and Fatality in Malaria-Endemic Regions - A Clue to Treatment?" (April 27), http://dx.doi.org/10.2139/ssrn.3586954. Virtually all arriving visitors to these African countries are taking a hydroxychloroquine-like quinolone drug for prophylaxis against malaria infection. About 70% of this antimalarial prophylaxis is thought to be atovaquone (Malarone). The initial observations made in April and reported about May 1, 2020, from the very preliminary data were that population-adjusted coronavirus fatality rate of industrialized West might be as high as one thousand times that of sub-Saharan Africa. Page 4. The coronavirus infection rate in the Industrialized West was thought to be as high as four hundred times greater than that for sub-Saharan Africa. Page 4. The death rate was felt to be more significant. Because this data was so preliminary, the article's conclusion was watered down considerably. The conclusion was that the preliminary data demonstrated a "wide (two orders of magnitude or one hundred-fold) disparity." Abstract, page 1. Continuing, those residing in "more affluent countries are about one hundred times more likely to become infected with coronavirus infection and die." Abstract, page 1. Those initial impressions have remains intact over the intervening six months. Second paper, ~ June 15, 2020. A second paper was written in mid-June, 2020. That paper sought to analyze some of the social determinants of disease and compare the high COVID death rate in New York City to another large crowded city in sub-Saharan Africa, Lagos, Nigeria - "A Tale of Two Cities - Lagos, Nigeria's apparent Success in the War Against COVID-19 (Crossover Prophylaxis Against Coronavirus by Antimalarial Agents)," http://dx.doi.org/10.2139/ssrn.3628644 That paper drew on data from European CDC and African sources as well as the Johns Hopkins Center for Systems Science and Engineering (CSSE) data used previously. The Lagos paper, like the first one, found that "a person's chances of dying from the coronavirus in this 2020 COVID-19 pandemic are more than six hundred times greater in New York City than in Lagos, Nigeria." "This dramatic disparity contradicts or at least diminishes the conventional wisdom that coronavirus mortality is exacerbated by city life, specifically poverty, overcrowding, racial differences, and diminished access to health care. The dramatic disparity in fatality rates between these two cities flies in the face of our traditional understanding of the social determinants of health." That paper concluded, "there is clearly a different factor at play here. These facts demand an explanation. This apparent protective effect conferred on those living in Lagos compared to New York City should be further analyzed for its etiology, significance, and potential benefit to others." Data Revisited, about August 1, 2020. The relevant SSA and U.S. mortality data was revisited in anticipation of a conference at the end of July. Three months after the first crossover prophylaxis article was published, and five months into the COVID pandemic, the two-hundred-fold population-adjusted fatality disparity remained intact. Data Revisited, about October 1, 2020 The relevant SSA and U.S. mortality data was revisited in anticipation of a conference in mid-October. Five months after the first crossover prophylaxis article was published, and seven months into the COVID pandemic, the two-hundred-fold population-adjusted fatality disparity was still intact at 214. At this point in time, in an effort to evaluate the best possible data, the data was age-adjusted for the percentage of a nation's population over 65 years of age. In Italy, 23% of the population is over 65. In the U.S. that figure is 16%. In the sub-Saharan African countries, the percentage of residents over 65 years of age is about 3%. When the population-adjusted fatality rates for the various countries are adjusted for ageadjusted for age, the U.S. and the industrialized West is still about thirty-seven times that of the six countries in Sub-Saharan Africa. It is imperative to note that the underlying mortality ratios have not changed. Age-adjusting the data was simply thought to be a more accurate way of representing it. At the same time the simple age-adjusted data set forth here on this website was verified by @CovidAnalysis at https://c19study.com/ using a more complex method. The results were virtually identical. The raw data has not changed. The initial population-adjusted data can be likewise retrospectively adjusted for age. Again, the trend and the underlying implications of the data are not changed. The age-adjusted fatality ratio for the U.S. and the industrialized West (Europe) remains nearly thirty-five times that of the six sub-Saharan African countries. Note that this is thirty-five times (3,400% more, not 35% more) the fatality rate in the six African countries, even after adjusting for age demographics. Also in October, a new data source was implemented. This was https://covid.ourworldindata.org/data/ecdc/total_deaths.csv. It is used to generate the long term graphs as opposed to the static point in time graphs previously generated with the Johns Hopkins Center for Systems Science and Engineering (CSSE) data. The Our-World-in-Data and the Hopkins CSSE data are remarkably consistent. Data Revisited, about November 1, 2020 Finally, the relevant SSA and U.S. mortality data was revisited around the first of November. This is now eight months into the pandemic and six months after the first crossover prophylaxis article was published. The two-hundred-fold population-adjusted fatality disparity and the age-adjusted fatality disparity remain intact. The SSA numbers have remained low and flat for six months, even as Europe and the U.S. are experiencing a spike in deaths and some European countries are entering new lockdowns. The initial claim of the first crossover prophylaxis article has remained solid over time. The graphic data speaks for itself. The Fatality rate for all six malaria-endemic sub-Saharan countries has remained low and astonishingly linear throughout the course of the pandemic. The raw, population-adjusted ratio of the fatality rates of the industrialized West has remained about 200 times that of the six malaria-endemic sub-Saharan African counties. This is clearly consistent with the "two orders of magnitude or one-hundred-fold disparity" asserted in the original article. The industrialized West has had 822 deaths per million population. The U.S. has had nearly a thousand death per million. For the six SSA countries, the figure is 28 COVID deaths per million inhabitants. The age-adjusted ratio has remained about thirty to thirty-five times greater in the U.S. and Western European countries compared to SSA for three months since it was first calculated. See the most current graph here. |